Equipping the Right Tools for Our AI Investigator Agent
by Yubin Park, Co-Founder / CTO
At Falcon Health, we recognized early that AI's greatest strength lies in expanding hypotheses and efficiently exploring new investigative angles. This insight led us to place AI-human collaboration at the center of our program integrity platform, ahead of the industry curve.
Our fraud, waste, and abuse (FWA) detection product, Sentinel, employs an AI investigator that works alongside human experts to generate new research angles, test theories against client data, analyze publicly available datasets, and explore complex data mappings. But as we refined our applications and tested against real-world scenarios, we discovered a critical gap: the AI needed specialized tools to effectively investigate healthcare fraud.
The Challenge: When Standard Search Falls Short
Consider a common investigative scenario: our AI needs to determine whether a specific procedure is covered for a particular medical condition. This requires checking National Coverage Determinations (NCDs) or Local Coverage Determinations (LCDs)—but anyone who has worked with these databases knows that conventional search methods simply don't cut it.
These are esoteric documents containing largely unstructured information. Some articles explicitly list specific HCPCS codes, others require particular lab values, and still others depend on diagnosis codes within claims data. While these documents make perfect clinical sense to healthcare professionals, they lack consistency and are notoriously difficult to parse and search programmatically.

Our Solution: Custom Domain-Driven Tools
Rather than accepting these limitations, we've spent months developing smart, specialized tools for our AI agent. Our flagship example: a completely restructured Medicare Coverage Determination database.
What we've built:
- Cleaned and structured data: We've transformed inconsistent policy documents into organized, searchable formats
- Code mapping: Each determination is populated with corresponding ICD-10 and HCPCS codes for precise matching
- Consistent organization: Standardized formatting eliminates the variability that confuses both AI and human investigators
- LLM-optimized summaries: Concise, structured information that prevents cognitive overload and reduces hallucination risk
Top tip
Here's the secret sauce: We don't just clean the data. We map every Medicare policy to actual billing codes (ICD-10, HCPCS) that appear in real claims. This turns fuzzy policy language into precise, searchable criteria that AI can actually use.
The Impact: Efficiency That Skyrockets
The results speak for themselves. Our AI investigator, equipped with these custom domain-driven tools, demonstrates dramatically improved performance:
- Faster resolution: Finds the right information without iterative back-and-forth queries
- Higher accuracy: Reaches correct conclusions without hallucinating false information
- Better focus: Stays on investigative course while exploring realistic hypotheses
- Deeper insights: Uncovers patterns that would be missed by traditional rule-based systems
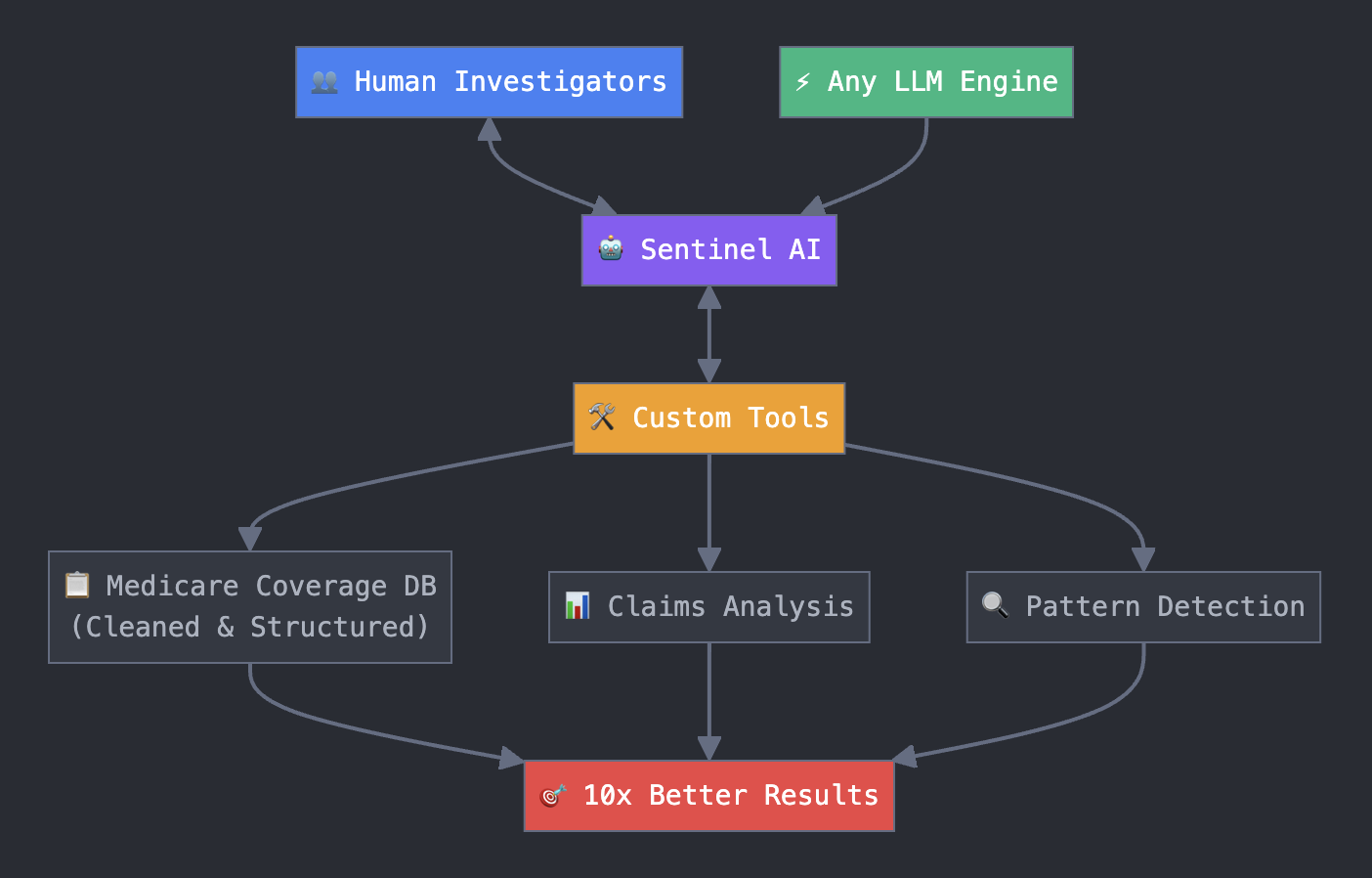
The Strategic Architecture: Future-Proof and Flexible
This tool-centric approach provides us with a crucial strategic advantage. Our framework allows us to upgrade our core AI engine independently from our specialized infrastructure. We can seamlessly integrate the world's best reasoning models as they emerge, while maintaining the sophisticated, domain-specific tools we've developed.
This separation means we're not locked into any single AI provider or model architecture. The competitive moat lies not in the underlying LLM, but in the years of work we've invested in creating tools that actually understand healthcare compliance, fraud detection, and program integrity.
Top tip
Think of it like this: Everyone's fighting over who has the fastest race car engine (LLM), while we're building the best pit crew tools. When the next engine comes out, we just swap it in, but our competitors still can't change their tires as fast.
Looking Forward: The Tool-Driven Future
We're continuing to develop additional specialized tools across the healthcare compliance landscape. Each tool we build deepens our platform's investigative capabilities and creates additional barriers for competitors trying to replicate our results.
At Falcon Health, we believe the future of AI in healthcare isn't just about having the smartest models. It's about equipping those models with the right tools to navigate the complex, nuanced world of healthcare data and regulation.
Interested in learning more about how Sentinel can transform your program integrity efforts? Visit us at falconhealth.ai or reach out to discuss how our AI-powered approach can enhance your fraud detection capabilities.